- Received November 19, 2022
- Accepted December 27, 2022
- Publication January 23, 2023
- Visibility 4 Views
- Downloads 0 Downloads
- DOI 10.18231/j.ijor.2022.019
-
CrossMark
- Citation
Long standing Brodie’s abscess of the diaphysis of the upper tibia in a young male
Introduction
The osteomyelitis is the inflammation of the bone and bone marrow caused by infection. Brodie's abscess is a subacute form of osteomyelitis which can last for many years without showing any signs of discomfort, and with normal test results. The metaphysis of the long bone is most commonly involved but it may involve diaphysis also. Most of the patients are between 10 to 20 years of age. The tibia is most commonly affected bone. Other less involved sites are fibula, femur, pelvic bone, radius, ulna, humerus, vertebra and cranium. Organisms of low virulence are believed to cause the lesion. Staphylococcus aureus is most common bacterium found in 50 percent culture of infected bone; and in 20 percent culture is negative. [1], [2]
Case Report
We present a case of a 21 years old male student with pain and swelling over right upper leg from 8 years. His pain and swelling became worse over the past few months. The pain was localized and non-radiating; aggravated on walking and relieved by taking rest and medication. He also gave a history of on and off fever and loss of appetite but denied any chills, night sweats and rashes. There was no history of previous trauma to the right lower limb.
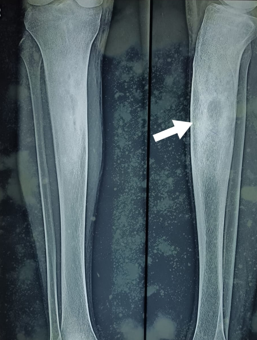
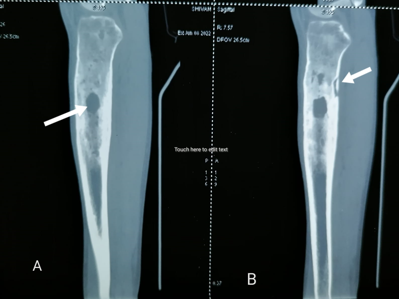
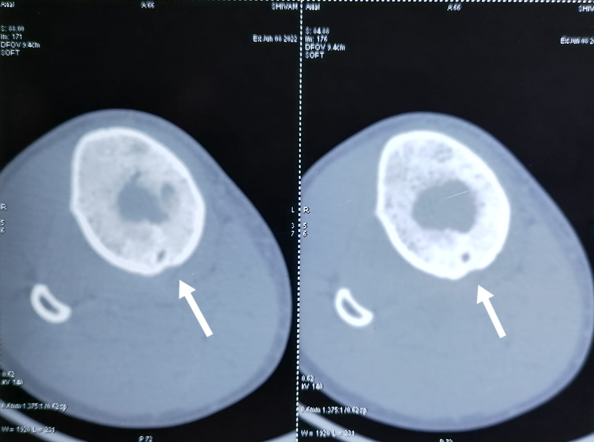
On examination the local temperature over the swelling was not raised but mild bony tenderness and cortical thickening were noticed over the proximal tibia. There was no discharging sinus or scar marks over the swelling. The routine blood tests revealed a normal white blood cell count, erythrocyte sedimentation rate and C reactive protein. On X-ray a large osteolytic lesion seen in the upper tibial diaphysis surrounded by a dense sclerotic bone with cortical thickening and periosteol reaction. No pathological fracture was seen and joint space normal ([Figure 1]). CT scan showed a well-defined osteolytic lesion with internal soft tissue density content and marked surrounding sclerosis in the upper part of the tibial diaphysis. There was a serpentine fistulous tract seen in the posterior aspect of this osteolytic lesion communicating with the adjacent soft tissue ([Figure 2]).
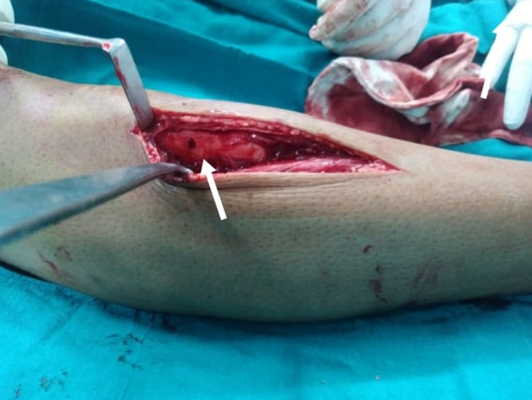
After anesthetic clearance the patient was planned for surgical exploration. The patient underwent bone drilling of the tibia wherein frank pus was noted within the medullary cavity. The fluid collection was irrigated thoroughly with normal saline and lesion was curetted completely and wound closed under drain ([Figure 3]). Histopathological evaluation revealed chronic granulomatous inflammation without any evidence of neoplastic pathology. Staphylococcus aureus grow in culture after 24 hours of incubation which was sensitive to cefazolin, cefixime, amoxicillin/clavulanic acid, azithromycin, cefuroxime and tetracycline. The intravenous antibiotics given for 2 weeks, after that oral antibiotics continued for another 6 to 8 weeks. Now the patient had no complaints of pain or any other symptom or recurrence.
Discussion
The osteomyelitis is known as the great imposter due to its ability to mimic various benign and malignant conditions, especially in its subacute and chronic states.[2] Sir Benjamin Brodie, a British surgeon first identified Brodie's abscess in a 24 years old man with persistent pain and swelling over the ankle in 1832. After the man's leg was amputated, it was discovered that the patient had a walnut-sized collection of dark coloured pus within the tibia.[3] Since its discovery low grade pyogenic abscess of bone has been referred as Brodie's abscess. Brodie's abscess is contained accumulation of pus in the bone, encircled by a rim of sclerosis which causes mildly suppressed systemic inflammatory response. This subtype of osteomyelitis has single focus of intraosseous abscess frequently with slow onset. Due to its subtle onset and limited systemic response high degree of suspicion required to diagnose this form of osteomyelitis.
It is not uncommon for surgeon to make an incorrect diagnosis or underdiagnosed the condition if sufficient imaging is not done. As much as 90% of cases are initially misdiagnosed; of the cases that are diagnosed, 50% are incorrectly diagnosed as tumours. [4]
Brodie's abscess typically affects the bones of lower limb with the tibia being involved more than the femur. Staphylococcus aureus is the pathogen that is most frequently found in the pus culture. Other less frequently encountered organisms are Streptococcus, Pseudomonas, Haemophilus influenza, Salmonella, Kingella kingae and coagulase-negative Staphylococcus aureus. Brodie's abscess is a hematogenous infection with predilection for metaphyses of long bones of lower extremity. Males affected more commonly than females with highest prevalence in patients below the age of 30 years. [5], [6], [7]
Patients frequently present with pain and swelling in the absence of fever and constitutional symptoms, making diagnosis difficult. The characteristic signs and symptoms of an acute osteomyelitis are absent. Typically WBC, ESR, and CRP are normal or slightly elevated. Blood culture is often negative. The most commonly used diagnostic modality is plain X-Ray. [8]
Brodie’s abscess can have clinical and radiological similarity to bone tumour making it difficult to diagnose. Osteoid osteoma is a benign bone tumor that most commonly affects long bones but may invade any bone. In a case report by Chan et al. he described the difficulty in distinguishing an osteoid osteoma from Brodie’s abscess radiographically. The abscess lesion is typically lucent and may vary in size from less than 1cm to more than 4cm in diameter with marginal sclerosis and cortical thickening. Although not pathognomonic, distinguished imaging features include a serpentine sinus tract, cloaca or soft tissue mass. Unlike benign bone tumour, the sequestrum of osteomyelitis is often eccentric and is within an irregularly marginated lucency, whereas osteoid osteomas consist of a central, round, smoothly-marginated calcification within a nidus of smooth inner margin.[2]
Other imaging modalities are CT scan and MRI, which provide additional information with further characterization of the lesions to support the findings of the X-Ray. Penumbra signs are typically confirming and aid in distinguishing neoplasm from osteomyelitis. [9], [10] The penumbra sign consists of subtle peripheral rim of high signal around the pus collection in bone on T1- weighted imaging. This high signal is caused by lipid laden macrophages in the granulation tissue of the abscess wall. [11]
The preferred method of treatment is open biopsy and curettage of the lesion, which is followed by intravenous and oral antibiotics. The optimal duration for which antibiotics is continued is still debatable. [12] Following surgical debridement, the diagnosis is confirmed by culture and histopathological analysis of pus.[13], [14]
Conclusion
Brodie’s abscess is a long standing localized form of osteomyelitis seen in cases where either the virulence of the infecting organism is low or the immunity of the host is good. The diagnosis is challenging and high degree of suspicion arises in this type of osteomyelitis. Imaging is essential in the work up of Brodie's abscess. CT scan and MRI are very useful and help in differentiating abscess from bone tumour. Surgical debridement followed by prolonged course of antibiotics is the preferred method of treatment and outcome is generally favourable.
Conflict of Interest
None.
Source of Funding
None.
References
- N Van Der Naald, D P Smeeing, R M Houwert. Brodie’s Abscess. A Systematic Review of Reported Cases. J Bone Joint Infect 2019. [Google Scholar] [Crossref]
- M Zairi, R Boussetta, A Msakni, A A Mohseni, M N Nessib. Subacute osteomyelitis of the tibial diaphysis associated with Brodie's abscess: A rare case report of a four-year-old child. Int J Surg Case Rep 2021. [Google Scholar] [Crossref]
- R Chan, B Abdullah, S Aik, C Tok. Radiofrequency ablation of a misdiagnosed Brodie’s abscess. Biomed Imaging Interv J 2011. [Google Scholar] [Crossref]
- BC Brodie. An account of some cases of chronic abscess of the tibia. Med Chir Trans 1832. [Google Scholar]
- Y Gulati, A V Maheshwari. Brodie's abscess of the femoral neck simulating osteoid osteoma. Acta Orthop Belg 2007. [Google Scholar]
- CE Foster, M Taylor, EK Schallert, S Rosenfeld, KY King. Brodie Abscess in Children: A 10-Year Single Institution Retrospective Review. Pediatr Infect Dis J 2019. [Google Scholar] [Crossref]
- AA Olasinde, KS Oluwadiya, OO Adegbehingbe. Treatment of Brodie's abscess: excellent results from curettage, bone grafting and antibiotics. Singapore Med J 2011. [Google Scholar]
- CS Hayes, SD Heinrich, R Craver, GD Macewen. Subacute osteomyelitis. Orthopedics 1990. [Google Scholar] [Crossref]
- SS Morgan, S Balasubramanian, D Teanby. Interesting clinical presentation of anterior knee pain causing diagnostic dilemma. Chir Organi Mov 2009. [Google Scholar] [Crossref]
- WB Morrison, ME Schweitzer, GW Bock, DG Mitchell, EL Hume, MN Pathria. Diagnosis of osteomyelitis: utility of fat-suppressed contrast-enhanced MR imaging. Radiology 1993. [Google Scholar] [Crossref]
- B Mcguinness, N Wilson, AJ Doyle. The "penumbra sign" on T1-weighted MRI for differentiating musculoskeletal infection from tumour. Skeletal Radiol 2007. [Google Scholar] [Crossref]
- P R Kornaat, M Camerlinck, F M Vanhoenacker, G De Praeter, HM Kroon. Brodie's abscess revisited. JBR-BTR 2010. [Google Scholar]
- BC Chen, T Kobayashi, H O'Rourke, P Sekar. Staphylococcus aureus osteomyelitis causing Brodie's abscess of the tibia in an adult man. BMJ Case Rep 2021. [Google Scholar] [Crossref]
- GS Dharmshaktu. Brodie’s abscess: Brief review of key updates from the year 2010. J Orthop Dis Traumatol 2020. [Google Scholar] [Crossref]
