- Visibility 11 Views
- Downloads 2 Downloads
- DOI 10.18231/j.ijor.2020.002
-
CrossMark
- Citation
Tuberculous pyomyositis of upper and lower limb muscles-A prospective study
- Author Details:
-
Javed Ahmad
-
Vivek Kumar Shrivastava
-
Ahmad Ayaz *
-
Anoop Raj Singh
-
Manis Khanna
Introduction
Extra-pulmonary tuberculosis is considered as a new disease due to its resurgence and increasing incidence in the twenty-first century, particularly in immuno-compromised patients.[1] About one-fifth of new diagnosed cases of tuberculosis have extrapulmonary lesion, of which about one-tenth involve the musculoskeletal system, arthritis, osteomyelitis and tubercular spondylitis. Tuberculous pyomyositis has been rarely described and its manifestations may mimic malignant tumour or other inflammatory disease as it presents as vague swelling.[2] There are various routes of involvement of skeletal muscles as contiguous spread from underlying bony infection (osteomyelitis), neighbouring joint or tendon sheaths, or from cold abscess, by direct inoculation (penetrating injury) and by haematogenous dissemination. Still the involvement of soft tissue by Mycobacterium tuberculae without underlying bony pathology is very rare and the pathogenesis is not well understood. [3]
Incidence of musculoskeletal tuberculosis occurs in only 3% of patients of all tubercular infections. Primary tuberculous pyomyositis is a rare infection constituting less than 1% of musculoskeletal tuberculosis. This can mimic inflammatory myositis or rarely mallignancy and can create diagnostic dilemma for orthopaedic surgeon. Mycobacterium tuberculae infection should always be considered as a rare but possible aetiology of myositis. Tuberculous pyomyositis in an immuno-competent patient without underlying bony involvement is an unusual presentation and its pathogenesis is still unclear.[2]
The route of infection was assumed to be one of three causes- ‘direct inoculation' if there had been a history of penetrating injury or surgery while the patient did not have pulmonary or other extra pulmonary tuberculosis, ‘contiguous spread’ if radiographic studies, revealed lesions in adjacent bone or soft tissues and ‘hematogenous’ in all other cases.[4]
Patients and Methods
The study was conducted at Mahamaya Rajkiya Allopathic Medical College, Ambedkar Nagar, on patients came to orthopaedic OPD during period between March-2012 to March-2019. It is a prospective study done on the OPD patients who came with complaints of pain, swelling with or without history of fever or trauma of both lower and upper limbs. Primarily they were diagnosed as soft tissue swelling, cold abscess or malignancy; on further evaluation, diagnosis was confirmed as Tubercular Pyomyositis.
Inclusion criteria
On the basis of observations we concluded the inclusion criteria which include both clinical and radiological parameters. Our inclusion criteria depend upon the following points-
Patients presented with pain and swelling of long duration of more than two months
Single swelling in the upper/lower limb
No raised local temperature on palpation of swelling
No redness or erythema of overlying skin
No discharging sinus
No bony involvement on X-ray
We framed the above inclusion criteria to rule out the common differential diagnosis like bacterial soft tissue infections and pyogenic abscess which presented with shorter duration of swelling with pain, temperature, fever and local soft tissue/bony tenderness. X-ray was done to exclude the common diagnosis like osteomyelitis and malignancy.
On the basis of above inclusion criteria we selected 28 patients and on further evaluations 16 patients diagnosed as tuberculous pyomyositis. During the study 2 patients had not visited for regular follow up.
There were 14 cases which included in this study. Among 14 cases there were 7 (50%) male and 7 (50%) female cases. The age of patients varied from 9 years to 68 years and the duration of illness at presentation in OPD from 2 months to 12 months. Out of 14 patients, 7 (50%) had problem in upper limb and 7(50%) in their lower limb.
Method of Evaluation and Management
Patients evaluated clinically followed by standard protocol as per suspicious swelling. All patients first evaluated clinically which includes history of contact of tuberculosis, duration of swelling, trauma and associated co-morbidities like diabetes mellitus, long standing steroid or immune-suppressant therapy, HIV infection. After that systemic and local examination was done on all the patients. The X-ray of the involved part was taken to look any pathology of the bone. Hematological parameters like haemoglobin, total leucocyte counts, differential leucocyte counts, blood sugar, ESR and CRP were done.
Ultrasonography (USG) was done to find out the nature of the swelling as solid or cystic, and to differentiate between superficial swellings of subcutaneous tissue from the deep swelling of muscle. Magnetic resonance imaging (MRI) was done to reveal the extension of the swelling of the involved muscle. For small swellings Fine Needle Aspiration Cytology (FNAC) was done. In large swelling aspiration was done with large bore needle and aspirate sent for gram staining, AFB staining, culture and sensitivity.
In very large swelling surgical drainage and debridement was done and tissue sent for histopathological examination. In some swelling biopsy was done to confirm the diagnosis. In all cases we had started symptomatic treatment from the first day visit in the form of NSAIDS, and once the diagnosis had been confirmed we started anti tubercular treatment (ATT) as per guideline of management of extra pulmonary tuberculosis for at least one year.
Patients having other co morbidities like diabetes mellitus as 2 of our patients, had continued the anti-diabetic drugs along with treatment of tubercular pyomyositis. All the managed patients doing well and they have taken their full course of ATT as per protocol till the last review.
| S.No | Age(y)/sex | Location | Duration on first presentation | MRI | Other comorbities | Route | Initial diagnosis | Management | Bony involvement |
| 1 | 9/m | Right proximal medial thigh | 4 months | 6x6x2cm, Adductor compartment | None | Hematogenous | Infection | Conservative | None |
| 2 | 22/f | Right distal arm posterioly | 3 months | 150x31x16mm, distal half of Triceps | None | Hematogenous | Cold abscess | Surgical | Superficial erosion of olecranon process |
| 3 | 24/f | Lateral aspect of right forearm | 4 months | 5x3x2cm,belly of Brachioradialis | None | Hematogenous | Infection | Surgical | None |
| 4 | 55/m | Right lower leg | 2 months | 6x6x4 cm of lower calf muscle | Diabeties mellitus | Direct (penetrating injury) | Infection | Surgical | None |
| 5 | 24/f | Lateral compartment of right thigh | 5 months | 185x31x69mm Vastus lateralis & intermedius | None | Hematogenous | Cold Abscess | Surgical | None |
| 6 | 60/m | Right proximal thigh | 7 months | 15x12x8 cm, Quadriceps Femoris | Pulmonary TB | Hematogenous | Cold Abscess | Surgical | None |
| 7 | 23/f | Anterior aspect of left forearm | 12 months | 8x4x2mm, Flexor digitorum superficialis | None | Hematogenous | Infection | Conservative | None |
| 8 | 68/f | Anterior & lateral aspect of left thigh | 7 months | 4x5x3 cm, Vastus lateralis & Vastus intermedius | Diabetes mellitus | Hematogenous | Malignancy | Conservative | None |
| 9 | 38/m | Anterior aspect of right forearm | 9 months | 55 x 28 x 26 mm, in the flexor compartment muscle | None | Direct (penetrating injury) | Infection | Surgical | None |
| 10 | 30/m | Left forefoot | 4 months | 22x16x8mm, flexor compartment muscles of foot | None | Direct (penetrating injury) | Infection | Surgical | None |
| 11 | 26/f | Lateral aspect of right forearm | 6 months | 5x3x2cm, belly of Brachioradialis | None | Hematogenous | Infection | Surgical | None |
| 12 | 12/m | Anterior aspect of left thigh | 4 months | 3x2x1 cm, Quadriceps femoris | None | Hematogenous | Mallignancy | Conservative | None |
| 13 | 55/m | Medial aspect of left thigh | 11 months | 6x3x3cm, Adductor muscle | None | Hmatogenous | Soft tissue tumor | Conservative | None |
| 14 | 36/f | Anterior aspect of proximal forearm right | 8 months | 3x4x2cm, Flexor compartment | None | Hematogenous | Swelling | Conservative | None |
Result
Management of tuberculosis is not a big issue in present scenario as we have different kind of anti-tubercular drugs and their protocol even for the resistant cases. The only problem is its proper diagnosis and mode of presentation. Tuberculous pyomyositis is a rare condition and mostly common in immuno-compromised patients but unfortunately it is not true with our study.
Depends upon their clinical presentation initially 28 cases were suspected among which 16 cases (57.10%) found positive for tuberculous pyomyositis. Two patients were lost during follow up, so finally there were 14 cases (50%) included in this study. Among 14 cases, 7 cases (50%) were female and 7 cases (50%) male. The age of patients varied from 9 year to 68 year and the duration of illness at presentation from 2 months to 12 months. The routes of infection were hematogenous in 11 cases (78.57%) and penetrating injury in 3 cases (21.42%). All cases were managed with ATT schedule as per guideline and surgery also needed in 8 cases (72.72%).
All the patients had received ATT for at least one year, and regular follow up was done up to six months after the completion of treatment. All the patients had developed some form of muscle contracture owing to disease of the muscle, for which we advised for physiotherapy.


Discussion
Pyomyositis is the bacterial infection of skeletal muscle with abscess formation, but when the causative micro-organism is Mycobacterium tuberculae, known as Tuberculous Pyomyositis. The real pathogenesis is still not clear but there are factors like penetrating injury, nutritional deficiencies, septic load, viral infections and parasitic infestations have been implicated as the predisposing factors.[4] Infection with Mycobacterium tuberculae is a rare cause of pyomyositis, particularly in immuno-competent patients as per literature but in endemic regions like India the pyomyositis may occur in a normal person. The rarity is also proven by literature as study done by J. Y. Wang et al. on 1153 suspects published in 2003; only 21 patients (1.8%) with culture-proven tuberculosis had tuberculous pyomyositis.[5]
Though the muscle involvement is rare in Mycobacterium tuberculae infection and there is possible explanations for the rarity of muscle involvement in tuberculosis include the high lactic acid content of the muscle, absence of lymphatic tissue and reticulo-endothelial tissue, well differentiated state of muscular tissue, and its good vascular supply.[6] The infection with Mycobacterium tuberculae bacilli involves a single large muscle, like quadriceps femoris, gastrocnemius, adductor longus/magnus, brachioradialis, flexor digitorum superficialis/profundus, biceps and triceps.
There are many explanations that the involvement of skeletal muscle is secondary to Mycobacterium tuberculae infection of underlying bones, synovial sheaths of nearby tubercular arthritis, by direct inoculation (penetrating injury) or hematogenous dissemination.[7] Just reverse to this concept some authors have reported tuberculosis of muscles as the primary site for infection.[8] In the absence of a direct spread from an adjacent primary focus, tuberculous pyomyositis may be found in penetrating injury, idiopathic in an immuno-competent host or there was no evidence of a tubercular focus elsewhere in the body as primary involvement.
Most common cause of tuberculous pyomyositis is typically caused by invasion from adjacent structures rather than by primary infection, hematogenous seeding or lymphatic spread[9] but in our study hematogenous spread was the most common route of infection. The prevalence of tuberculous pyomyositis is more common in immuno-deficient patients and associated with the use of corticosteroids, the presence of HIV infection, the administration of cancer chemotherapy, and renal failure.[10]
There are many case reports in literature supporting this evidence like a case report presented by Siao-pin Simon et al. reported a 66 year old female patient on immuno-depressent therapy presents with tuberculous pyomyositis of her right thigh muscle;[11] and by Pradeep Khandalvalli et al. presented a case report in 2019 of an immuno-compromised patients, a 35 year old female renal allograft recipient presented with multiple subcutaneous abscess involving left forearm, left thigh, suture site and left loin, which on later evaluation revealed to be due to Mycobacterium tuberculae.[12]
Tuberculous pyomyositis can develop in immuno-competent persons, with the common symptoms of Mycobacterium tuberculae infection such as evening rise of temperature, night sweats, malaise, loss of appetite, and weight loss.[13]
The diagnosis of tuberculous pyomyositis is still mostly based on clinical suspicion such as its insidious onset, slow progression, non-responsiveness to various antibiotics, and by its responsiveness to anti-tubercular chemotherapy retrospectively, as described in literature but many times only a vague swelling of long duration is the only presentation. The typical symptoms are more common in immuno-compromised patients as compared to immuno-competent patients as per literature. There are differential diagnosis which includes bacterial, fungal, or tuberculous abscesses, hematoma and neoplasm.[14]
A positive tuberculin test only helps as a guide to the suspicion of Mycobacterium tuberculae infection but may not be positive always. Demonstration of acid-fast bacilli (AFB) on Ziehl– Neelsen stain from the aspirate from swelling may further confirm the etiology. However this may not be true in some cases if the bacterial load in the abscess is low. In such cases, the aspirate may be negative for AFB stain despite the abscess being of Mycobacterium tuberculae infection. A pathological report of granulomatous inflammation is beneficial in the early diagnosis of tuberculous pyomyositis, even if the AFB stain is negative. That is why we had advised for all patients FNAC and aspiration, and in some cases histopathological evaluation was done in which AFB staining failed to demonstrate acid fast bacilli.[15]
On hematological evaluation laboratory parameters in patients with tuberculous pyomyositis may include low haemoglobin, leukocytosis, an elevated erythrocyte sedimentation rate (ESR), and elevated creatine phosphokinase (CPK) levels, though none of these is specific to this particular diagnosis and none are seen in each case.[16]
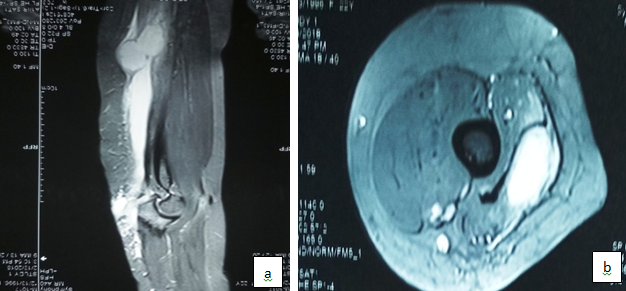
Imaging modalities such as ultrasonography (USG), computed tomography scan (CT scan), and MRI is important in diagnosing pyomyositis. The location, extent, and consistency of a swelling can be determined by these imaging studies, which aid the process of establishing a differential diagnosis of tuberculous pyomyositis. We did USG and MRI for all of our cases to know the extent of involvement of infection.[17]
MRI is the best modality for evaluating soft-tissue masses, including inflammatory infectious processes. Still, when T1- and T2-weighted images are used, it is sometimes difficult or even impossible to differentiate neoplastic (benign or malignant) from non-neoplastic swellings, including inflammatory swellings. MRI helps well to establish the extent of involvement of bone. There was no bony involvement except superficial bony erosion in one of our case on MRI. The small areas of relatively low signal intensity within the abscess on the T2-weighted images generally represent necrotic material and proteinaceous debris. [18]
Pyomyositis, which is due to pyogenic bacterial organisms, has three clinical stages-[19]
Invasive stage- clinical symptoms are mild with pain, fever, and anorexia, the disease being in a subacute form.
Suppurative stage- high grade fever, chills, myalgia, septic syndrome and fluctuation in the muscle due to the presence of pus.
Stage of systemic manifestations- sepsis and fever with possibility of complications like metastatic abscesses, arthritis, septic shock and renal failure.
Treatment of pyomyositis is surgical drainage or USG/CT-guided drainage of the abscesses with administration of appropriate intravenous antibiotics. Pyomyositis of tubercular origin is comparatively rare and does not follow the classical three stages of pyogenic pyomyositis. The literatures have reported few cases of tuberculous pyomyositis treated with surgical drainage and debridement, with recurrence requiring further surgeries.[18], [20]
There is no specific guideline for the management of tuberculous pyomyositis, though the cornerstone happens to be early diagnosis and anti-tubercular chemotherapy.[21]
Effective drainage of the abscess must be ensured by aspiration or by surgical exploration. The surgical option may be reserved for the following conditions, such as – [22], [23]
A rapid enlarging painful swelling acting as space-occupying lesions and causing jeopardization of other functional structures in the vicinity.
Recurrence after aspiration or debridement
Immuno-compromised state, where the bacterial load is high
Associated with bony erosion
A Doubtful diagnosis.
Non-responsiveness to anti-tubercular drugs despite culture being positive for Mycobacterium tuberculae
Failed aspiration of the abscess and thereby lack of effective drainage
A high level of clinical suspicion supplemented with mycobacteriological testing and relevant imaging study is necessary to make an early diagnosis of tuberculous pyomyositis. In most cases, receiving timely diagnosis, effective drainage, and appropriate anti-tubercular chemotherapy, the prognosis for functional recovery is good.
There are few limitations of our study like there is no immuno-compromised patients in this study as the patients included in this study are selected randomly on the basis of our inclusion criteria. Tubercular pyomyositis is a rare disease so it needs a long duration for study for example as in literature a retrospective study was done by J. Y. Wang et al. on 1153 suspects published in 2003 the duration from January 1996 to March 2001, but only 21 (1.8%) patients had diagnosis of tuberculous pyomyositis,[5] and in our study during the period of March 2012 to March 2019 total 28 patients initially selected on the basis of our inclusion criteria among which 14 (50%) patients found to be tuberculous pyomyositis. This is the limitation of our study and is due to the small number of patients; but on other side it also proves the efficacy of our inclusion criteria as there were 50% of suspects had tuberculous pyomyositis.
Conclusion
Isolated presentation of tuberculosis as pyomyositis is rare and not widely reported in the literature. Tuberculous pyomyositis should be considered in long standing vague swelling of the upper and lower limb without constitutional symptoms and signs of inflammations. Thus it is our recommendation is to establish the diagnosis of tubercular pyomyositis followed by anti tubercular treatment; and in selected cases surgical drainage and debridement along with ATT.
Consent
The written and informed consent was obtained from the every patient for the publication of this paper and any accompanying images.
Source of Funding
None.
Conflict of Interests
None.
References
- Mpe Puttik, H B Stein, Rmt Chann, R K Elwood, A R How, G D Reid. Soft tissue tuberculosis: a series of 11 cases. J Rheumatol 1995. [Google Scholar]
- S Batra, M Ab Naell, C Barwick, R Kanvinde, . Tuberculous pyomyositis of the thigh masquerading as malignancy with concomitant tuberculous flexor tenosynovitis and dactylitis of the hand: Case Report. Singapore Med J 2007. [Google Scholar]
- Jacques Pouchot, Philippe Vinceneux, Janine Barge, Françoise Laparee, Yves Boussougant, Christopher Michon. Tuberculous polymyositis in HIV infection. Am J Med 1990. [Google Scholar]
- K L Huang, D M Chang, J J Lu. Tuberculosis of skeletal muscle in a case of polymyositis. Scand J Rheumatol 1999. [Google Scholar]
- J Y Wang, L N Lee, P R Hsueh, J Y Shih, Y L Chang, P C Yang. Tuberculous myositis: a rare but existing clinical entity. Rheumatol 2003. [Google Scholar]
- O Baylon, B Demiralp, E I Cicek. A case of tuberculous pyomyositis that caused a recurrent soft tissue lesion localized at the forearm. Jpn J Infec Dis 2002. [Google Scholar]
- Vivek Trikha, Vikas Gupta. Isolated Tuberculous Abscess in Biceps Brachii Muscle of a Young Male. J Infect 2002. [Google Scholar]
- A G Kulkarni, S A Julkarni. Primary intramuscular cold abscess in the left deltoid region: a case report. East Afr Med J 1990. [Google Scholar]
- Jamil Ahmed, James Homans. Tuberculous pyomyositis of the soleus muscle in a fifteen-year-old boy. The Pediatric Infectious Disease Journal 2002. [Google Scholar] [Crossref]
- Funda Ergin, Hande Arslan, Banu Bilezikçi, A. Muhteşem Ağildere, Nurhan Özdemir. Primary Tuberculosis in the Gluteal Muscle of a Patient with Chronic Renal Failure. Nephron 2001. [Google Scholar]
- Daniela Siao-Pin Simon, Daniela Fodor, Raluca Valasciuc, Maria-Magdalena Tamas, Simona Rednic. A rare case of primary tuberculous pyomyositis .Case Report. Med Ultrason 2011. [Google Scholar]
- Manjusha Yadav, Pradeep Khandalvalli, Shabana Nazneen. An unusual clinical presentation of tuberculous pyomyositis in a renal allograft recipient. Saudi J Kidney Dis Transpl 2019. [Google Scholar]
- Jerome H. Kim, Sara Wallerstein, Marla Thoe, Anita Wolfe, Darrell Rask. Myopathy in Tuberculosis: Two Presumptive Cases and a Review of the Literature. Mil Med 1997. [Google Scholar]
- P Mootsikapun, A Mahakkanukrauh, S Suwannaroj. Tuberculous pyomyositis. J Med Assoc Thai 2003. [Google Scholar]
- M. J. Ashworth, T. H. Meadows. Isolated Tuberculosis of a Skeletal Muscle. J Hand Surg [Br] 1992. [Google Scholar]
- I.D. Bobrowitz. Active tuberculosis undiagnosed until autopsy. Am J Med 1982. [Google Scholar]
- C K Chu, T L Yang, C T Tan. Tuberculous pyomyositis of the temporal muscle in a non immune-compromised woman: diagnosis by sonography. J Laryngol Otol 2004. [Google Scholar]
- H. Paajanen, W. Grodd, D. Revel, B. Engelstad, R.C. Brasch. Gadolinium-DTPA enhanced MR imaging of intramuscular abscesses. Magn Reson Imaging 1987. [Google Scholar]
- O Baylan, B Demiralp, E I Cicek. A case of tuberculous pyomyositis that caused a recurrent soft tissue lesion localized at the forearm. Jpn J Infect Dis 2005. [Google Scholar]
- J Y Wang, L N Lee, P R Hsueh. Tuberculous myositis: a rare but existing clinical entity. Rheumatol 2003. [Google Scholar]
- E.-Y. Jang, S.-O. Lee, S.-H. Choi, H. Sung, M.-N. Kim, B.-J. Kim. Case of Pyomyositis Due to Mycobacterium haemophilum in a Renal Transplant Recipient. J Clin Microbiol 2007. [Google Scholar]
- R D Farnell, N Davies, A J Unwin. Tuberculous compartment syndrome of the forearm. Orthop 2001. [Google Scholar]
- J C George, K A Buckwalter, E M Braunstein. Tuberculosis presenting as a soft tissue forearm mass in a patient with a negative tuberculin skin test. Case report. Skeletal Radiol 1994. [Google Scholar]
